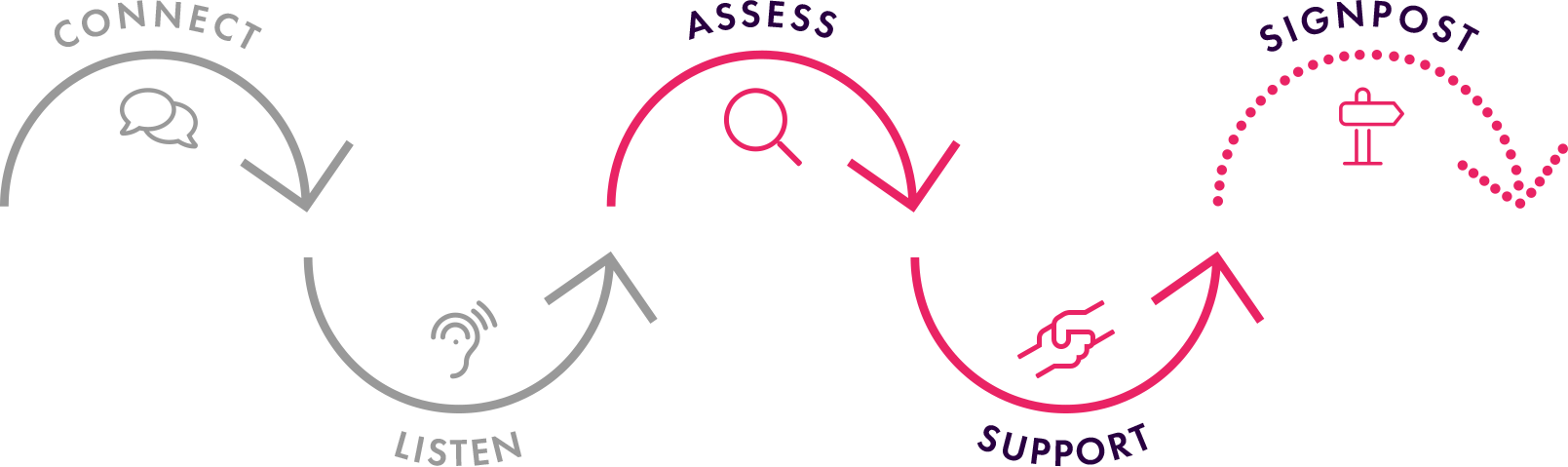
Whilst in the listening phase, we are also assessing the person’s safety. If you spot the warning signs, risk factors and see the individual in distress then ask them directly whether they are having any thoughts about ending their life (after connecting and listening to them). On some occasions, after connecting with them they may open up without the question being asked.
It is a myth to think by asking this question you are putting the thought into their head. If the individual states they are not having these thoughts, offer them support.
If they are experiencing suicidal thoughts, find out whether they have any intentions , protective factors , and any preparations in place to end their life.
 Low Risk
Low Risk
- No intentions
- Protective factors
- Stable situation
Support:
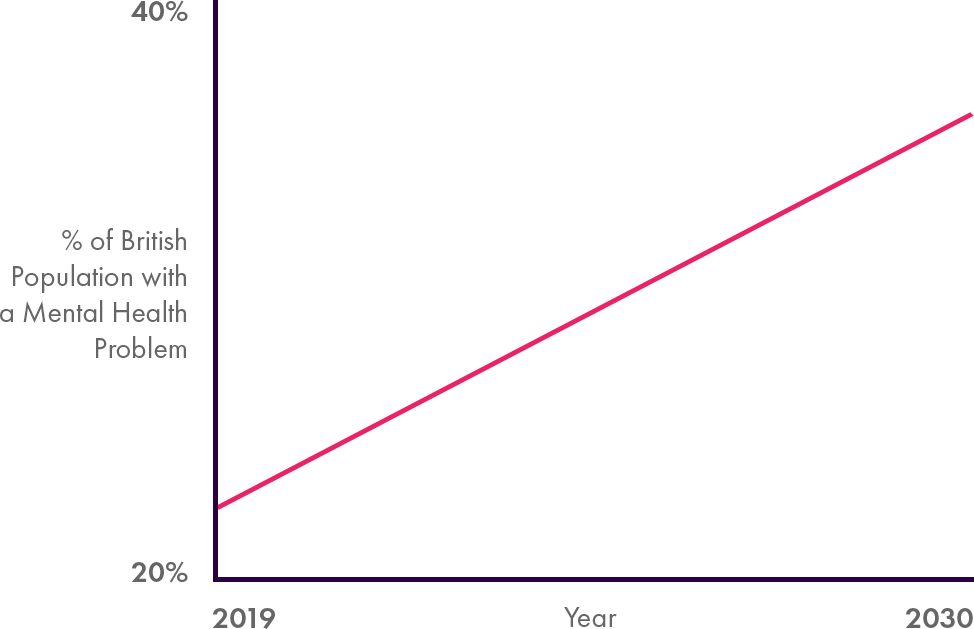
Offer your support and normalise feelings of suicide (20.6% of the British population have had suicidal thoughts in their lifetime). State that you are here for them.
Signpost:
Encourage your colleague to visit their GP. Also state that Samaritans 24/7 who run a confidential helpline (116 123) or they can call and ambulance or visit out of hours GP if the situation becomes more severe.
 Moderate Risk
Moderate Risk
- Intentions to end life
- Protective factors
- Situation vulnerable to change
Support:
Offer your support and normalise feelings of suicide (20.6% of the British population have had suicidal thoughts in their lifetime). State that you are here for them.
Signpost:
Encourage your colleague to visit their GP. Also state that Samaritans 24/7 who run a confidential helpline (116 123) or they can call and ambulance or visit out of hours GP if the situation becomes more severe.
 High Risk
High Risk
- Intentions to end life
- No protective factors
- Preparations to end life
Support:
Don’t leave the individual. Comfort and empathise with them.
Signpost:
Either request an emergency out of hours GP appointment or call an ambulance (999)